Every July, thousands of newly minted doctors begin their residency training programs across the United States. This year, a time that is usually filled with excitement and anticipation — the thrill of new ID badges that say “physician” and fresh, long white coats — will now collide with an incredibly tumultuous political landscape that will impact generations of physicians. In some states, it will also affect the at least 1 in 4 women who, before Roe v. Wade was struck down by the Supreme Court, were likely to have an induced abortion during their reproductive years.
Almost half of the nation’s OG/GYN residency programs are in states that have or will ban abortions, which will create crucial gaps in medical education.
Almost half of the nation’s OB-GYN residency programs are in states that have or will ban abortions, which will create crucial gaps in medical education. This, in turn, will make access to equitable, high-quality reproductive health care impossible, or severely lacking, for patients.
Medicine is a highly regulated profession, with licensing boards, state medical boards and detailed educational standards. Within hours of the Supreme Court decision, the Accreditation Council for Graduate Medical Education, the body responsible for accrediting all residency programs in the United States, proposed modified language, stating:
“Obstetrics and gynecology residency programs may be located in jurisdictions where there are legal restrictions on induced abortions. Requirements have been added for programs in jurisdictions where there are such restrictions. These requirements preserve the goal of training competent obstetrician/gynecologists to be able to provide comprehensive reproductive health care.”

But how these requirements will be implemented remains unclear.
In Louisiana, 4 of 5 residency programs contract with one abortion clinic that now faces an uncertain future and may have to shut down, which would leave those residents without requisite education. Oklahoma’s two medical schools currently do not offer abortion training, which forces medical students and residents to find other opportunities to understand important components of clinical care. Physicians in Wisconsin overwhelmingly support abortion training but now face potential issues recruiting students and residents into obstetrics and gynecology programs due to a possible lack of clinical and teaching experience.
Abortion training is broad and includes learning how to perform dilation of the cervix and surgical evacuation of the uterus after the first trimester of pregnancy, medical abortions, and medical management of miscarriages. Research shows that abortion training improves general reproductive health skills and improves the quality of other obstetric procedures.
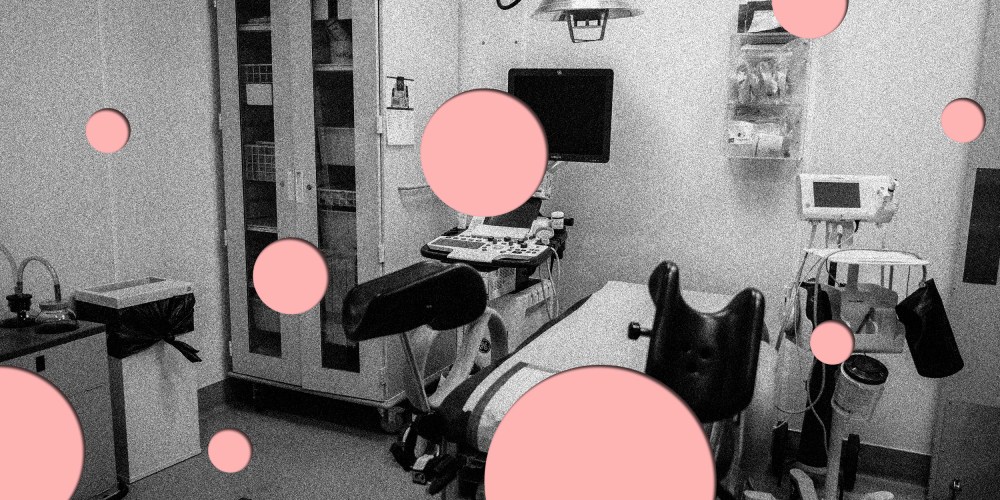
Along with the technical aspects of training, there is an incredible amount of education during the “in between” time — counseling a patient prior to their decision, helping them with the incredible emotions that occur throughout and humanizing the sterile environment of the clinic and procedure room. Understanding aspects of trauma-informed care enhances the compassion in medicine and underscores the “care” part of health care.
Research shows that abortion training improves general reproductive health skills and improves the quality of other obstetric procedures.
Training programs can send residents to other states, but they will then have to face simultaneous workforce shortages in their own institutions. Physicians do not train in isolation; they hold their residencies and practice all across the country, so physicians who do not receive training and therefore cannot recognize certain health conditions could easily end up in the other America, where reproductive justice has been upheld and for which they will be unequipped. Unfortunately, if the doctor who sees you has little to no experience, it is likely no better than being in a state where abortion is banned.